What All Women Should Know About Mammograms
Radiologist, Deaconess Breast Services10/09/2019
As a specialist in breast cancer detection, I know a lot about mammograms.I work full time in Deaconess Breast Services, reviewing mammograms and breast MRIs, performing biopsies, and working closely with staff to help women find breast cancer at its earliest, most treatable stages.
Breast cancer will develop in 1 in 8 American women in her lifetime, so it’s very important that women be informed about options and recommendations for early detection. Unfortunately, there is no guaranteed way to prevent breast cancer. However, if breast cancer is found early—before it spreads to other areas of the body– 98% of women will survive a breast cancer diagnosis.
Regular screening mammograms are still the best way to find breast cancer early, which means that mammograms are the best tool in the fight against breast cancer. I know that there is some confusion regarding mammogram recommendations, so I want to address that. I’m also going to explain what 3D mammography is, and why it’s the superior choice for women.
What is a mammogram and when should I have one?
A mammogram is an x-ray picture of the breast. Mammograms can be used to check for breast cancer in women who have no signs or symptoms of disease. This type of mammogram is called a screening mammogram, which typically includes 2 or more images of each breast. The x-ray images often make it possible to detect tumors that cannot be felt.
There are some organizations that have said women who are of average risk for developing breast cancer can delay screening mammograms until later in their 40s, or even to age 50. I disagree with that.
I’m a member of the American College of Radiology (ACR), and the Society of Breast Imaging. Both of these professional, medical organizations recommend that women of average risk (more on that in a bit) should have an annual screening mammogram starting at age 40.
Unfortunately, I have seen many women diagnosed with breast cancer in their early 40s. If they would’ve waited until age 45 or even 50 for a screening mammogram, their cancers wouldn’t have been detected until a more advanced stage.  While it is true that the vast majority of breast cancers are diagnosed in women over 50, women who develop breast cancer at younger ages often have a more aggressive type of cancer, which is more dangerous because it spreads more quickly.
For reference, here are details of the official position of the ACR.
Are there specific reasons to have a mammogram before age 40?
Women who have a history of breast cancer in their family (mother, sister, grandmother, daughter) may be at an increased risk for breast cancer, especially if their relative was diagnosed at an early age (before 50), or if multiple blood relatives have had breast cancer.
If you have this kind of family history, talk with your primary care doctor and/or your OB/GYN about what screenings may be right for you. Sometimes a woman with a family history of breast cancer should begin annual screening mammograms at an age that is 10 years younger than when the family member was diagnosed. Some women may benefit from breast MRI screenings. Any screening outside the general guidelines will require a physician order, so your doctor is your partner in making this decision.
Additionally, women with dense breasts (as determined by their first mammogram) may also benefit from a modified screening plan, which should be discussed with their doctor.
Finally, any woman who notices something abnormal about her breasts (such as a lump, dimple/puckering, leaking from the nipple, etc.) should notify her doctor immediately. A diagnostic mammogram may be needed. A diagnostic mammogram is used to closely look at breast abnormalities and is not the same as a screening mammogram.
What are the risk factors for breast cancer? Â
The list below from the CDC is a comprehensive list of risk factors for breast cancer. Studies have shown that a woman’s risk for breast cancer is due to a combination of factors.
The main factors that influence your risk include being a woman and getting older, as most breast cancers are found in women who are age 50 or older. Some women will get breast cancer even without any known risk factors besides being a woman and over 50.
Having a risk factor does not mean you will get the disease, and not all risk factors have the same effect. Most women have some risk factors, but most women do not get breast cancer. If you have breast cancer risk factors, talk with your doctor about ways you can lower your risk and about screening for breast cancer.
Risk factors include
- Getting older. The risk for breast cancer increases with age; most breast cancers are diagnosed after age 50.
- Genetic mutations. Inherited changes (mutations) to certain genes, such as BRCA1 and BRCA2. Women who have inherited these genetic changes are at higher risk of breast and ovarian cancer.
- Early menstrual period. Women who start their periods before age 12 are exposed to hormones longer, raising the risk for breast cancer by a small amount.
- Late or no pregnancy. Having the first pregnancy after age 30 and never having a full-term pregnancy can raise breast cancer risk.
- Starting menopause after age 55. Like starting one’s period early, being exposed to estrogen hormones for a longer time later in life also raises the risk of breast cancer.
- Not being physically active. Women who are not physically active have a higher risk of getting breast cancer.
- Being overweight or obese after menopause. Older women who are overweight or obese have a higher risk of getting breast cancer than those at a normal weight.
- Having dense breasts. Dense breasts have more connective tissue than fatty tissue, which can sometimes make it hard to see tumors on a mammogram. Women with dense breasts are more likely to get breast cancer.
- Using combination hormone therapy. Taking hormones to replace missing estrogen and progesterone in menopause for more than five years raises the risk for breast cancer. The hormones that have been shown to increase risk are estrogen and progestin when taken together.
- Taking oral contraceptives (birth control pills). Certain forms of oral contraceptive pills have been found to raise breast cancer risk.
- Personal history of breast cancer. Women who have had breast cancer are more likely to get breast cancer a second time.
- Personal history of certain non-cancerous breast diseases. Some non-cancerous breast diseases such as atypical hyperplasia or lobular carcinoma in situ are associated with a higher risk of getting breast cancer.
- Family history of breast cancer. A woman’s risk for breast cancer is higher if she has a mother, sister, or daughter (first-degree relative) or multiple family members on either her mother’s or father’s side of the family who have had breast cancer. Having a first-degree male relative with breast cancer also raises a woman’s risk.
- Previous treatment using radiation therapy. Women who had radiation therapy to the chest or breasts (like for treatment of Hodgkin’s lymphoma) before age 30 have a higher risk of getting breast cancer later in life.
- Women who took the drug diethylstilbestrol (DES), which was given to some pregnant women in the United States between 1940 and 1971 to prevent miscarriage, have a higher risk. Women whose mothers took DES while pregnant with them are also at risk.
- Drinking alcohol. Studies show that a woman’s risk for breast cancer increases with the more alcohol she drinks.
Research suggests that other factors such as smoking, being exposed to chemicals that can cause cancer, and night shift work may also increase breast cancer risk.
We recommend an excellent self-assessment tool for determining your personal lifetime risk for breast cancer. We encourage you to take this test and discuss the results with your physician.
What is 3D mammography?
Mammography, and in particular, 3D digital mammography, is the gold standard in breast cancer screening.
In 2D imaging, cancerous tumors can be hidden behind normal breast structures. That’s because photos of the breast are taken looking all the way through the breast in one view.
3D mammography, also called tomosynthesis, helps radiologists see clearer, more detailed photos of the breasts. The mammography machine takes images of the breasts in layers, helping us see the breast in clearer, more precise views. Imagine a loaf of bread—a 2D image takes a photo of the whole loaf in one photo. A 3D image is like slices of the loaf, helping us see abnormalities much more easily.
In a 2D mammogram, if there appears to be an area of concern, the doctor may want to further investigate with another mammogram or a biopsy. Looking at the same breast tissue in visual “slices†from the 3D mammogram exam, the doctor can now determine if the tissue is in fact normal breast tissue creating the illusion of an abnormal area. This helps reduce call-backs and biopsies.
Have a look at the images below for comparison.
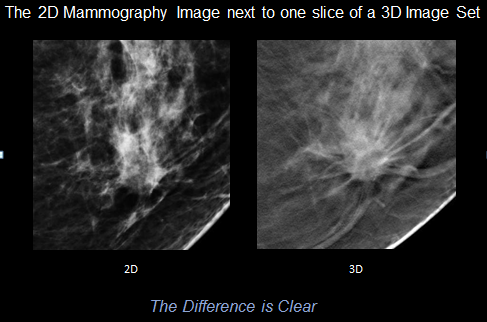  In this image, there is a gathering of tissue or “thickening†on the 2D mammogram that isn’t completely clear. However, in the 3D image, a lump is clearly seen—a lump that is cancerous.
 In this image, there is a gathering of tissue or “thickening†on the 2D mammogram that isn’t completely clear. However, in the 3D image, a lump is clearly seen—a lump that is cancerous.
As you can see in the 2D image below, a bright mass appears to be present at the front of the breast, which would have likely resulted in the woman having additional imaging or possibly a biopsy. But as you can see in the 3D image slides, that bright spot was normal breast tissue that was “stacked,†making it look like there was something there that really wasn’t.
Deaconess Breast Services is the only breast screening organization in the Tri-State to receive designation as a Breast Imaging Center of Excellence by the American College of Radiology (ACR). We’re very proud of this designation, as it means that our breast imaging centers have earned accreditation in mammography, stereotactic breast biopsy, and breast ultrasound (including ultrasound-guided breast biopsy), and breast MRI.
We offer 3D mammography at all three of our screening locations, including:
- Deaconess Breast Center at Deaconess Midtown
- The Breast Center at The Women’s Hospital
- The Mobile Breast Center
By ensuring that we are the highest-rated Breast Imaging Center in the tri-state, Deaconess Breast Services is doing everything we can to help win the fight against breast cancer.
There are additional Deaconess services related to breast cancer that we believe women should know about. Â
Genetic counseling
If you have a family history of breast cancer, you may benefit from oncology genetic counseling. The Women’s Cancer Center, located in the Chancellor Center for Oncology, offers the expertise of the only oncology genetic counselor in the entire region.Â
Certain people may benefit from meeting with an oncology genetic counselor, such as those with a personal and/or family history of:
- Early-onset cancers, usually diagnosed before age 50
- Cancer in two or more first-degree relatives on the same side of the family (maternal or paternal history)
- Multiple primary tumors (more than one type of cancer in one individual)
- Bilateral tumors (affecting, for example, both breasts or both ovaries)
- A relative who is a known carrier of an inherited cancer gene
Contact The Women’s Cancer Center to learn more.
Multidisciplinary Breast Cancer Clinic
When a woman is diagnosed with breast cancer, having a team of cancer experts can improve outcomes. The Multidisciplinary Breast Cancer Clinic involves multiple physicians and experts to create a personalized treatment plan for each patient.
Mobile Breast Center
We’re proud to have recently completed a full year of bringing 3D mammograms to women throughout the region via the Deaconess Mobile Breast Center. See where screening mammograms will be offered close to you.
Convenient mammogram scheduling
When you make the decision to have your annual screening mammogram, we can provide your screening and results the same day. You don’t need to wait for an appointment either! Schedule your mammogram online–right now–or simply call 812-450-6266.




