Otters mount eighth inning comeback over Crushers
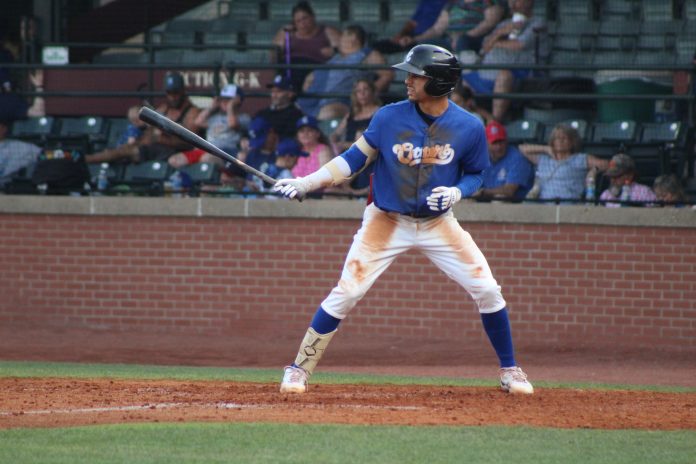
The Otters trailed by a run entering the eighth. Jomar Reyes led off with a base hit and after two straight outs, George Callil worked a walk.
Rosario then blasted a ball off the glove of the Crushers’ left fielder to plate both runs and give Evansville the lead.
A Kona Quiggle single scored Rosario to bring the Otters’ lead to two runs.
Jake Polancic worked around a leadoff single and a walk to secure the Evansville victory. The closer earned his ninth save of the season, tied for the most in the Frontier League.
Jeffrey Baez opened the Evansville scoring, hitting a two-run homer over the left field wall in the third inning. The slugger leads the team with 13 homers.
Quiggle joined the power party with a solo home run in the fourth inning to extend the lead to 3-0.
Lake Erie responded with a solo home run in the fifth inning. They took the lead with four hits in the sixth inning, good for three runs and a 4-3 lead.
Starting pitcher Tim Holdgrafer did not factor into the decision. He retired the first eight batters of the game.
Holdgrafer finished with 5.1 innings pitched, allowing four runs on six hits with six strikeouts.
Evansville’s bullpen allowed just three baserunners over 2.2 innings. Jon Beymer pitched four outs. Kevin Davis worked an in-order eighth inning.
Quiggle finished with three hits, two runs and two RBIs. Reyes added three hits including a double.
The win is Evansville’s first victory when trailing after the seventh inning or later this season.
The Otters and Crushers play the middle game of the series Wednesday evening with a 6:35 PM CT first pitch from Bosse Field. Senior fans can enjoy discounted senior GA tickets as part of a Senior Connection Wednesday.
Indiana State Police Seeks Recruits for the Capitol Police Section
The Indiana State Police Capitol Police Section is accepting applications.  Individuals interested in beginning a rewarding career as a Capitol Police Officer may apply online at https://www.Capitol Police Career Opportunities. This website provides a detailed synopsis of the application process and information on additional career opportunities with the Indiana State Police Department.
Applications must be submitted electronically by 11:59 pm (EST) on Wednesday, August 9, 2023.
Basic Eligibility Requirements and consideration factors for a Capitol Police Officer:
- Must be a United States citizen.
- Must be at least 21 years of age when appointed as a police employee.(Graduation date is December 15, 2023)
- Must meet a minimum vision standard (corrected or uncorrected) of 20/50 acuity in each eye and 20/50 distant binocular acuity in both eyes.
- Must possess a valid driver’s license to operate an automobile.
- Must be a high school graduate as evidenced by a diploma or general equivalency diploma (GED).
The academy begins on Monday, October 23, 2023.  The starting salary for a Capitol Police Probationary Officer is $62,327 a year.  After the first year of employment, the salary will increase to $64,472.00.  The Indiana State Police Capitol Police Section also offers an excellent health care plan, including medical, dental, vision, and pharmacy coverage for current and retired employees and their families.  The State maintains short-term and long-term disability plans for full time employees after six (6) months of continuous employment.  As an Indiana State Police Capitol Police Officer, you are automatically enrolled in the Public Employees Retirement Fund (PERF), and the State will contribute to your retirement account.
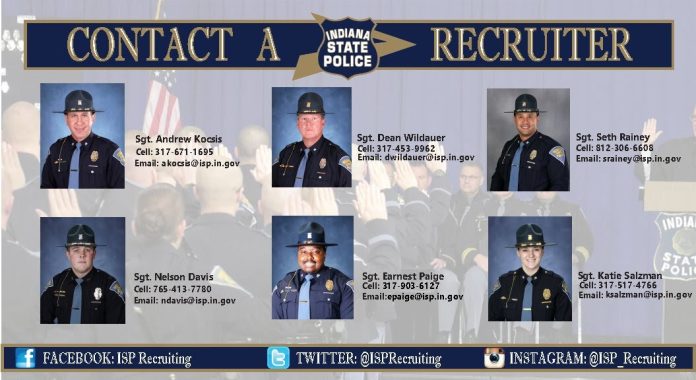
Interested applicants can obtain additional information about a career as a Capitol Police Officer by visiting https://www.Capitol Police Career Opportunities. Applicants can also contact a recruiter at isprecruiting@isp.in.gov.
PHE funds may have overpaid hospitals, study suggests
PHE funds may have overpaid hospitals, study suggests
Public health emergency funding during the COVID-19 pandemic helped hospitals’ net operating margins hit an all-time high, according to a study published in JAMA Health Forum July 14.
The study examined national RAND data and American Community Survey data between 2017 and 2021 to evaluate hospitals’ financial performance during the first two years of the COVID-19 public health emergency. Researchers assessed 4,423 short-term acute care and critical access hospitals.
Eighty percent of the hospitals received public health emergency funds during 2020 and 2021. Seventy-five percent had a positive net operating income during this period. For more than 3,000 hospitals, financial performance improved post-public health emergency; these facilities saw a median net operating income improvement of $5.3 million.
Median operating margins reached an all-time high of 6.5 percent between 2020 and 2021, compared with 2.8 percent margins pre-2020 according to the study. Hospitals saw a median $1.9 million increase in net operating income during this time period.
However, 16 percent of hospitals experienced new financial distress despite receiving public health emergency funding. Nearly one-fifth of the hospitals were located in a census tract with more than 20 percent Hispanic residents; these facilities were more likely to experience financial distress even after receiving federal funds. A high concentration of Hispanic residents was the only independent variable associated with financial distress after receipt of public health emergency funding, according to the study.
And not all funds were distributed equally, the study pointed out. Hospitals with uncompensated care that represented 10 percent or more of their operating expenses in 2019 were less likely to receive COVID-19 funding than those that reported no uncompensated care burden.
Highly urban hospitals averaged $4.8 million more in COVID-19 funding than rural hospitals and health system-affiliated hospitals received $1.2 million less than unaffiliated hospitals. For-profit hospitals received $5.4 million less than nor-for-profit hospitals, but still were not in financial distress during the emergency, according to the study.
Some relief funds went to hospitals that did not need them while others received too much, the study’s authors noted in their discussion. This led some hospitals to hit peak operating margins rather than restore to pre-pandemic levels.
“It should be underscored that policymakers were required to act quickly to direct COVID-19 PHE funding; however, based on the COVID-19 lessons, it will be important to consider alternative ways of allocating scarce public dollars to support our nation’s health system in crisis,” the authors wrote. “To that end, policymakers should ensure they have the necessary data to estimate the effects and to proactively build models to simulate relief payments and their effects on hospital finances, which could be used to better inform decision-making regarding the allocation of emergency aid.”