“Indiana is now the national leader in reforming the broken health care system and lowering prices.”
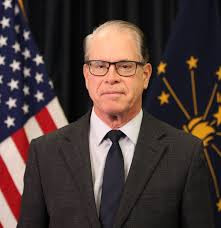
INDIANAPOLIS – Today, Governor Mike Braun held a ceremony to sign 10 health care bills that will bring substantial reform to health care in Indiana: lowering prices, leading the nation in health care price transparency, and eliminating the anti-competitive practices and misaligned incentives that drive up hospital prices, among many other notable health care solutions.
“I promised Hoosiers I would take on the big health care industry and get solutions to the problems making health care unaffordable. My partners in the General Assembly and I have enacted landmark health care solutions to bring transparency, accountability, and competition to our health care system. Indiana is now the national leader in health care reform and lowering prices for patients.” — Governor Mike Braun
Governor Mike Braun stated in his first State of the State address that health care reform for Hoosiers would be a top priority of his Freedom and Opportunity agenda this legislative session.
The bills celebrated today address systemic problems with the health care industry with solutions like full hospital price transparency so patients know what something costs upfront, ending anticompetitive practices in physician non-compete agreements to increase market competition, reforming how pharmacy benefit managers operate to drive down prescription drug prices, establishing that health plan administrators have a fiduciary duty to act in the best interest of the patients they act on behalf of, and ensuring that nonprofit hospitals actually act like nonprofits with new accountability measures.
Laws celebrated:
HEA 1003, Patient-centric, landmark health care solutions package
This patient-centric, landmark legislation was one of Governor Braun’s priority agenda bills and incorporates a number of provisions intended to bring transparency, accountability, and enforcement mechanisms to the health care industry. Specifically, this legislation:
- Requires nonprofit hospitals with a net patient revenue above $2 billion to apply Site of Service payments to outpatient office settings located off-campus from a hospital. This will ensure that outpatient facilities are only charging professional fees for providing health care services to Hoosiers enrolled in Medicaid or commercial insurance plans;
- Empowers Hoosiers with rare and terminal diseases by expanding Indiana’s right to try statute to include individualized treatments;
- Codified federal protections against surprise medical bills and clarified enforcement authorities available to the State;
- Prohibits insurers from denying coverage for eligible care on the basis that the patient was referred by an independent or out-of-network provider;
- Clarified that patients and employers have an absolute right to access their health information and claims data at no cost;
- Reduced the turnaround time from 5 days to 48 hours in which providers and insurers must provide a good faith estimate for a patient’s anticipated out-of-pocket costs for the services scheduled for the patient’s in-patient or out-patient treatment; and
- Empowers the Indiana Attorney general to designate law enforcement officers within the Medicaid fraud control unit to investigate waste, fraud, and abuse, as well as develop improved intra-government data sharing standards to support investigating alleged overpayments, duplicative claims, and claims or billings detected through the State’s fraud detection process.
HEA 1004, Lowering hospital prices for Hoosier patients
This legislation introduces a number of initiatives aimed at lowering hospital costs and addressing Medicaid financing and reimbursement, including:
- Hospital cost transparency
- Requires a nonprofit hospital system to submit audited financial statements and provides for a $10,000 per day penalty for failure to submit the statements to the state
- Requires the office of management and budget to develop a methodology to be used in conducting a study of commercial inpatient hospital prices and outpatient hospital prices and to determine Indiana’s statewide average inpatient and outpatient hospital prices
- By 2029, requires an Indiana nonprofit hospital system’s aggregate average inpatient and outpatient hospital prices to at least be equal to or less than the statewide average.
- Established a Medicaid state directed payment program for hospitals
- Directed payments to be included in the managed care capitation rates (not separate payment term)
- Allows FSSA to designate provider classes in a way to incentivize hospitals to lower ACR and using data from the hospital audited financial statements submitted to the state
- Established a managed care assessment fee
- Allows for FSSA to submit a request for a tax waiver for the creation of the assessment fee
- The assessment fee may be used to fund the Medicaid program
- Revises disproportionate share (DSH) payments
- Pauses most DSH payments when a state directed payment program is in effect
- Allows FSSA to submit a SPA to develop and implement DSH payments for state
SEA 2, Making Medicaid more sustainable
This legislation creates several Medicaid reforms around eligibility, reporting, work requirements and presumptive eligibility.
SEA 3, Fiduciary Duty in Health Plan Administration
This legislation requires pharmacy benefit managers (PBMs) and third party administrators (TPAs) to have a fiduciary duty to the plan sponsor that the PBM or TPA is acting on behalf of. Fiduciary duty obligates PBMs and TPAs to:
- Allows FSSA to submit a SPA to develop and implement DSH payments for state
- Act with loyalty and care in the best interest of the plan sponsor;
- Ensure all fees, costs, and commissions are disclosed to the plan sponsor;
- Avoid self-dealing and conflicts of interest; and
- Maintain transparency in all financial and contractual arrangements related to the plan sponsor’s health insurance coverage, including prescription drug benefits.
SEA 140, Reforming Pharmacy Benefit Managers
This legislation prohibits PBMs from utilizing anti-competitive contracting and business practices against pharmacies, including retroactively denying, reducing reimbursement, or seeking refunds or recoupments for a dispensing claim paid to a pharmacy, penalizing a pharmacy for selling a lower cost alternative to an insurer, limiting or preventing a patient from obtaining medication from a non-affiliated pharmacy, including specialty drugs, discriminating against pharmacies located within the health plan’s geographic coverage area and is willing to participating in the health plan’s network, including all-or-nothing clauses in contracts with pharmacies to require additional contracting with affiliates of the insurer, PBM, or administrator, and reimbursing a pharmacy at a net amount that is either less than what the insurer or PBM would reimburse itself or an affiliated pharmacy for the same prescription drug by national drug code number or the national average drug acquisition cost (NADAC) plus a fair pharmacy dispensing fee.
SEA 118, 340B Drug Program Report
This legislation requires covered entities participating in the 340B Discount Drug Program, as well as contract pharmacies and child sites, to annually report certain information and financial transactions to the Indiana Department of Health (IDOH). Failure to report the required information will result in the issuance of a civil monetary penalty of $1,000 per day.
SEA 475, Ending anti-competitive practices in physician noncompete agreements
This legislation prohibits hospitals, including a parent company or affiliated manager of a hospital and hospital systems, from requiring a physician to enter a noncompete agreement after July 1, 2025.
HEA 1604, Cost Sharing; Out-of-Pocket Expense Credit
This legislation requires health plans to credit the amount paid for a lower cost, out-of-pocket health care service towards and individual’s deductible, regardless of whether the service was provided by an in-network or out-of-network provider. Additionally, insurers and health plan administrators are required to apply the annual cost sharing limitation prescribed under the Patient Protection and Affordable Care Act for prescription drugs that are covered under the health plan, are life-saving or intended to manage chronic pain, and do not have an approved generic equivalent.
HEA 1666, Ownership of Health Care Providers
This legislation requires hospitals, insurers, PBMs, TPAs, and entities that accept Medicaid and Medicare to report ownership information to the State, and authorizes the Indiana Attorney General to investigate market concentration of a health care entity and review the ownership information submitted to the State.
SEA 480, Prior Authorization
This legislation revises Indiana’s prior authorization regulatory framework to better protect the provider-patient treatment plan and timely access to care.